(阅读笔记)急性卒中CT灌注分析在临床中的实际问题
- Introduction
- Understanding the basics of CTP acquisition and processing
- CTP thresholds and quantification
- Pitfalls of perfusion imaging
- Technical pitfalls
- Patient motion
- Contrast bolus
- Radiation
- Clinical pitfalls
- Core volume measurement errors
- Misclassification of ischemic penumbra (hypoperfusion)
- Stroke mimics
- Perfusion in posterior circulation and lacunar infarcts
- MRP
- Future directions
- Conclusion
期刊文献《Automated CT perfusion imaging for acute ischemic stroke:Pearls and pitfalls for real-world use》阅读笔记。
目前只是翻译了其中重要内容,尚未整理


Introduction
Many stroke centers are quickly incorporating the use of automated perfusion processing software to interpret perfusion raw data.
许多中风中心正在迅速使用自动灌注处理软件来解释灌注原始数据。
As CT perfusion (CTP) is being assimilated in real-world clinical practice, it is essential to understand the basics of perfusion acquisition, quantification, and interpretation.
随着CT灌注(CTP)在现实世界的临床实践中被吸收,了解灌注采集、量化和解释的基本知识至关重要。
It is equally important to recognize the common technical and clinical diagnostic challenges of automated CTP including ischemic core and penumbral misclassifications that could result in underestimation or overestimation of the core and penumbra volumes.
同样重要的是,认识到自动CTP的常见技术和临床诊断挑战,包括缺血核心和半影错误分类,这可能导致低估或高估核心和半暗带体积。
Two randomized trials (DAWN and DEFUSE 3) have thrust acute cerebral perfusion imaging into the routine evaluation of acute ischemic stroke with large vessel occlusion (i.e., intracranial internal carotid artery [ICA] or middle cerebral artery trunk [M1]) with definitive data.
两项随机试验(DAWN和DEFUSE 3)将急性脑灌注成像纳入了对大血管闭塞(即颅内颈内动脉[ICA]或大脑中动脉主干[M1])急性缺血性卒中的常规评估,并提供了明确的数据。
CTP data with manual postprocessing requires an active user interface to get adequate quantitative evaluation and may add interobserver variability. However, even with the use of fully automated software to process CTP results, clinicians have a significant learning curve to interpret the output data accurately.
具有手动后处理的CTP数据需要一个活跃的用户界面来获得足够的定量评估,并可能增加观察者之间的可变性。然而,即使使用完全自动化的软件来处理CTP结果,临床医生也有一条重要的学习曲线来准确地解释输出数据。7
This review is written to aid the acute stroke clinician, who must interpret data output from automated perfusion post processing software, in the real-world emergency setting to make time-dependent treatment decisions in the setting of acute ischemic stroke.
本综述旨在帮助急性中风临床医生在真实世界的紧急情况下解释自动灌注后处理软件的数据输出,以在急性缺血性中风的情况下做出与时间相关的治疗决策。
Understanding the basics of CTP acquisition and processing
了解CTP获取和处理的基础知识
CTP consists of a temporal sequence of images obtained during the wash-in and the wash-out of an IV bolus of iodinated contrast agent.
CTP包括在碘化造影剂的IV团的冲洗和冲洗期间获得的图像的时间序列。
For each pixel on a CTP map, hemodynamic parameters are calculated based on the time-density curves created from the wash-in and the wash-out of contrast material in this pixel.
对于CTP图上的每个像素,血流动力学参数是根据该像素中造影剂的冲洗和冲洗产生的时间密度曲线计算的。
- 到达最大值的时间(Tmax或延迟时间)表示从扫描开始到造影剂团的最大强度到达每个体素的时间。它是以秒表示的绝对值。
- 平均通过时间(MTT)表示造影剂团穿过体素所需的平均时间,以秒为单位测量。MTT与脑灌注压力成反比,在正常组织中通常持续约4-5秒。10
- CBF是指在单位时间内以脑质量为单位流动的血液体积,单位为毫升/100克/分钟(mL/100克/分)。正常灰质的CBF(约80mL/100g/min)高于正常白质(约20ml/100g/min)。10
- CBV指的是脑血容量,相当于包含血管的体素的分数,8–10以单位mL/100g表示。注意,参数CBF、MTT和CBV在数学上由以下等式关联:CBF=CBV/MTT,这也被称为中心体积原理。11因此,这些参数中的任何2个的测量足以导出第三参数。
The time-density curves, and specifically the area under the curve, of each voxel are influenced by 2 major factors: (1) arterial flow (i.e., the arterial input function) and (2) the tissue itself (i.e., its inherent hemodynamic properties).
每个体素的时间密度曲线,特别是曲线下面积,受到两个主要因素的影响:(1)动脉流量(即动脉输入功能)和(2)组织本身(即其固有的血流动力学特性)。
Numerous factors can alter the temporal profile of arterial flow of contrast agent delivery to tissue, resulting in delay, or dispersion, of the contrast bolus; examples include impaired cardiac output, ca rotid artery stenosis, and injection-related factors such as the injection rate and the saline chase.
许多因素可以改变向组织输送造影剂的动脉血流的时间分布,导致造影剂推注的延迟或分散;示例包括心输出量受损、ca rotid动脉狭窄和注射相关因素,如注射速率和盐水追逐。
To minimize the effect of the temporal profile of arterial flow on time-density curves, a mathematical operation called deconvolution is performed to show the true hemodynamic properties of the tissue being depicted.
为了最小化动脉血流的时间分布对时间密度曲线的影响,进行了一种称为去卷积的数学运算,以显示所描绘组织的真实血流动力学特性。
CTP thresholds and quantification
Pitfalls of perfusion imaging
下面我们将重点介绍常见的技术和诊断缺陷以及识别和应对这些问题的实用策略。
Technical pitfalls
技术缺陷
The importance of optimizing the technical acquisition of a perfusion study cannot be overstated.
优化灌注研究技术获取的重要性怎么强调都不为过。
It is difficult for any perfusion software to sufficiently correct an inherently poor acquisition using a postprocessing algorithm;
任何灌注软件都很难使用后处理算法充分校正固有的不良采集;
“garbage in, garbage out.”
“垃圾进来,垃圾出去。”
Assessing image quality metrics from a technical standpoint should be the first step in CTP interpretation and should be performed before evaluating the color and quanti tative perfusion maps.
从技术角度评估图像质量指标应该是CTP解释的第一步,并且应该在评估彩色和定量灌注图之前进行。
Patient motion
Because of the cine acquisition (i.e., dynamic successive gantry rotations), even slight motion can degrade a perfusion study.
由于电影采集(即动态连续机架旋转),即使轻微的运动也会降低灌注研究。
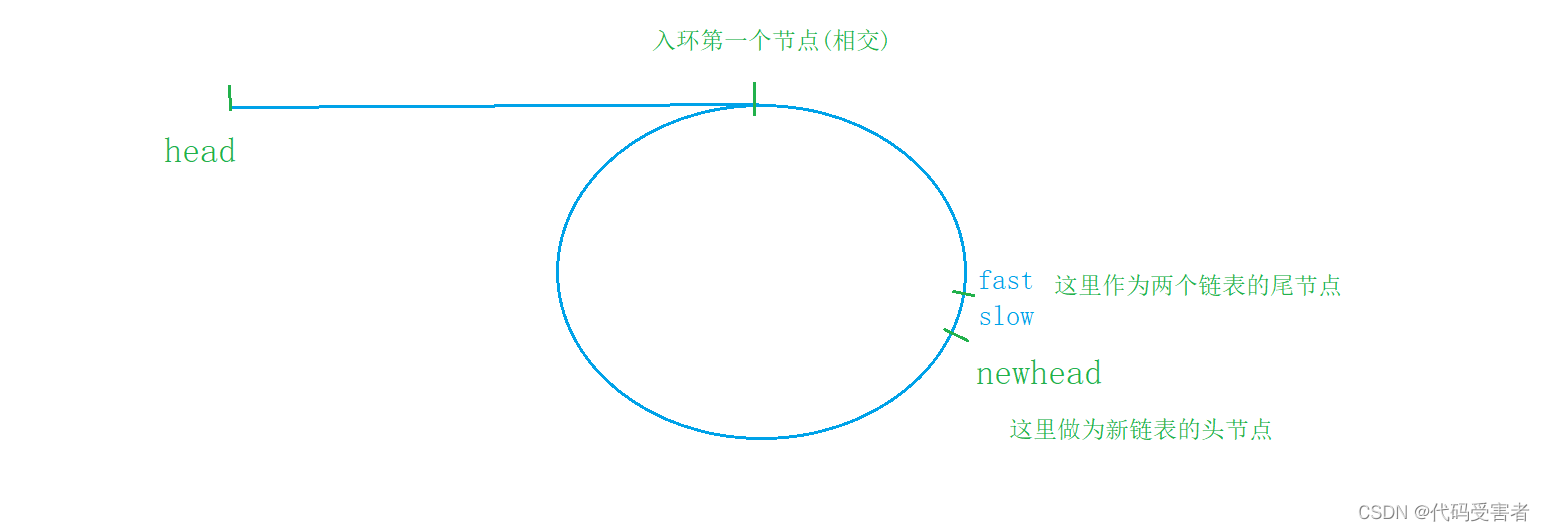
The majority of automated software packages routinely provide patient motion profiles, which provide a graphical estimate of rotational and translational motion (figure 2).
大多数自动化软件包通常提供患者运动轮廓,提供旋转和平移运动的图形估计(图2)。
We recommend routinely checking the patient motion profile in the automated report and, in cases with severe motion, potentially repeating the perfusion study with appropriate head immobilization (e.g., taping).
我们建议在自动报告中定期检查患者的运动情况,如果运动严重,可能会通过适当的头部固定(例如,胶带)重复灌注研究。
It is also important to scan the patient with the head in a symmetrical position without head tilt.
同样重要的是,在患者头部处于对称位置且不倾斜头部的情况下进行扫描。
The CTP software uses the contralateral side as reference for detecting the core, and spurious asymmetry between the brain hemispheres could lead to incorrect results.
CTP软件使用对侧作为检测核心的参考,大脑半球之间的虚假不对称可能会导致错误的结果。
Also, with angulation or head tilt, the distance of the axial slice of the brain will be at unequal distance from the major arterial supply, potentially leading to false penumbra.
此外,在成角度或头部倾斜的情况下,大脑轴向切片与主要动脉供应的距离将不相等,这可能导致假半影。
Contrast bolus
Contrast bolus characteristics, particularly duration of contrast administration, ensure adequate cerebral saturation of iodinated contrast in cerebral tissue.
对比剂推注的特点,特别是对比剂给药的持续时间,确保了脑组织中碘化对比剂的充分脑饱和。
A scan duration of ;70 seconds, which covers both wash-in and wash-out of contrast bolus, is usually sufficient to accurately assess the ischemic lesion volumes.28
扫描持续时间:;70秒,包括造影剂推注的冲洗和冲洗,通常足以准确评估缺血病变体积。28
Importantly, in patients with large vessel occlusions, however, contrast arrival may be delayed, and the CTP scan may end earlier than appropriate (i.e., truncation).
然而,重要的是,在大血管闭塞的患者中,造影剂的到达可能会延迟,CTP扫描可能会提前结束(即截断)。
The ideal time-density curve (figure 2) should not have any early truncation or incomplete wash-out and an adequate baseline period of image acquisition (representing no contrast initiated yet).
理想的时间密度曲线(图2)不应具有任何早期截断或不完全冲洗,以及足够的图像采集基线周期(表示尚未启动对比度)。
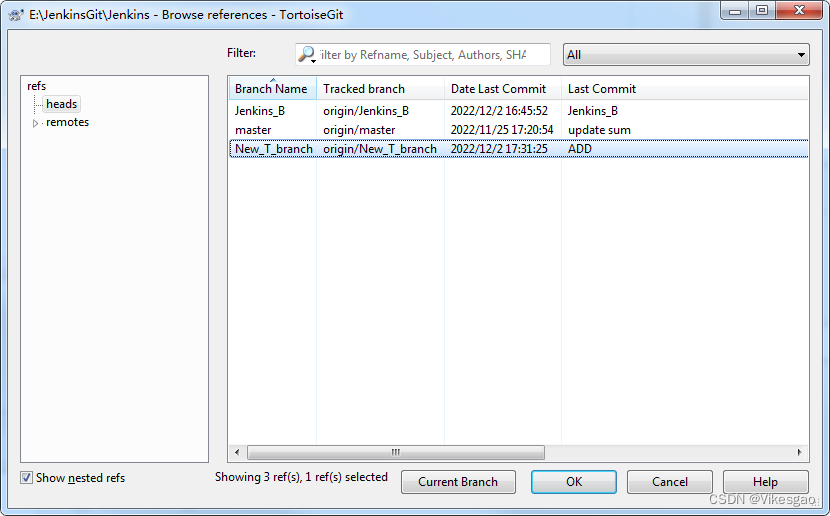
In addition, inadequate IV access, such as a distal/hand IV or small IV bore, can also contribute to an insufficient bolus profile (figure 3);
此外,静脉注射通路不足,如远端/手部静脉注射或小静脉注射孔,也可能导致推注轮廓不足(图3);
a contrast injection rate of at least 4 mL/min is recommended for proper CTP acquisition.
对于正确的CTP采集,推荐至少4mL/min的造影剂注射速率。
Nontechnical factors that can affect contrast bolus characteristics include comorbidities of low cardiac output, atrial fibrillation, cardiac arrhythmias, aortic dissection, severe proximal ICA stenosis, and ICA dissection; interpretation should be more tentative in the setting of these comorbidities.
可影响造影剂推注特征的非技术因素包括低心排血量、心房颤动、心律失常、主动脉夹层、严重的近端ICA狭窄和ICA夹层的合并症;在这些合并症的背景下,解释应该更具试探性。
Radiation
CTP acquisition involves repeatedly scanning the head for 60–70 seconds, resulting in relatively high radiation doses that typically equate to an additional noncontrast CT scan.
CTP采集涉及重复扫描头部60–70秒,导致相对较高的辐射剂量,通常相当于额外的非扫描CT扫描。
Moreover, erroneous CTP protocols could increase the dose to the organs, including skin and ocular lens by 3- to 11-fold.29
此外,错误的CTP方案可能会使包括皮肤和眼晶状体在内的器官的剂量增加3至11倍。
FDA investigations30 of highly publicized incidents31 of ra diation overdose from CTP in the acute stroke setting have led to well-established recommendations for CTP protocols.
美国食品和药物管理局(FDA)对在急性中风环境中因CTP引起的辐射过量的事件进行了调查30,并对CTP方案提出了完善的建议。
The technique should typically use a low peak tube potential of 80 kVp32 and tube current of 100–200 mAs.33 Additional information on technical acquisition pitfalls is available in data available from Dryad (additional information, doi.org/10.5061/dryad.b9q0dg4).
该技术通常应使用80 kVp32的低峰值管电位和100–200 mAs的管电流。33 Dryad提供的数据中提供了关于技术采购陷阱的更多信息(更多信息,doi.org/10.5061/Dryad.b9q0dg4)。
Clinical pitfalls
Core volume measurement errors
缺血核心的自动体积计算通常基于预定义的阈值;例如,大多数软件包将CBF相对减少70%的脑组织识别为缺血核心。23在一项评估CTP性能的研究中,RAPID CTP后处理算法显示,与预测DWI最终梗死的rCBF<38%(95%对87%)相比,rCBF阈值<30%更高具有更高的特异性。24最近对第二个队列(SWIFT PRIME数据库)中使用RAPID预测最终梗死体积的不同阈值的准确性进行的分析34表明,仅在少数情况下,常用的rCBF阈值<30%核心体积。这项研究还提出了一个替代的rCBV阈值0.32,其绝对误差中值与rCBF 30%相似,但高估了中值堆芯的体积。3
Conventional thresholds were derived from large data sets, with an emphasis of being more inclusive inpatient selection (i.e., allowing more underestimation rather than over estimation of core volumes). Therefore, individual patient predictions will not vary in accuracy.
传统阈值来源于大型数据集,强调更具包容性的住院患者选择(即,允许更多的低估而不是过度估计核心容量)。因此,个体患者预测的准确性不会发生变化。
For example, the ischemic core (defined by MRI-DWI) may not be identified in the automated outputs resulting in underestimation of the core if the reduced CBF of the acute infarct has not reached the predefined threshold in an individual patient.
例如,如果急性梗死的CBF降低未达到单个患者的预定义阈值,则可能无法在自动输出中识别缺血核心(由MRI-DWI定义),从而导致低估核心。
This could also be related to the timing of the CTP acquisition in relation to stroke onset and whether reperfusion therapies have been used.
这也可能与CTP采集的时间与中风发作以及是否使用了再灌注疗法有关。
In the extended time window, the ischemic core may be underestimated on CTP outputs if leptomeningeal collaterals have resulted in partial reperfusion of completely infarcted tissue.
在延长的时间窗内,如果软脑膜侧支导致完全梗死组织的部分再灌注,则可能低估缺血核心的CTP输出。
Therefore, it is critical to always assess the noncontrast CT; the presence of clear hypodensity on CT (low ASPECTS), if larger than seen as the predicted core on CTP, should always be taken into account.
因此,始终评估非扫描CT至关重要;如果CT上存在明显的低密度(低ASPECTS),如果大于CTP上预测的核心,则应始终考虑。
A clear hypodensity on noncontrast CT is consistent with the ischemic core, even if not defined by the CTP. Computed tomography angiogram (CTA) source images can also sometimes demonstrate clear hypodensity and should be assessed.
即使CTP未定义,非扫描CT上的明显低密度与缺血核心一致。计算机断层摄影血管造影(CTA)源图像有时也会显示明显的低密度,应进行评估。
The authors also suggest futuristic CTP summary maps with a 3-color “traffic light” output for the ischemic core and penumbra based on different thresholds for rapid vs delayed reperfusion
作者还提出了未来的CTP总结图,根据快速和延迟再灌注的不同阈值,为缺血核心和半影提供了三色“红绿灯”输出
Misclassification of ischemic penumbra (hypoperfusion)
Ischemic penumbra may be misclassified due to either technical or flow-related patterns.
缺血性半影可能因技术或血流相关模式而被错误分类。
The most common location of overcall in penumbral measurement is seen at the base of the skull, posterior fossa, or orbits (figure 3) and is relatively easy to recognize.
在半影测量中,最常见的覆盖位置是颅底、后颅窝或眼眶(图3),相对容易识别。
In a multisite study, the interpreting neurologists easily recognized hypoperfusion abnormalities as artifacts in skull base and orbits.36
在一项多站点研究中,解释神经科医生很容易将低灌注异常识别为颅底和眼眶的伪影。
However, the total penumbral volume calculation produced by the software still includes these arti facts, a potential source of overestimation of penumbral volume.
然而,该软件产生的总半影体积计算仍然包括这些人工因素,这是高估半影体积的潜在来源。
Other scenarios of overcalling ischemic penumbra include limitations to arterial flow, such as chronic carotid stenosis, low cardiac output, cardiac arrhythmia, previously discussed.
缺血半影过多的其他情况包括动脉血流受限,如慢性颈动脉狭窄、低心排血量、心律失常,如前所述。
Penumbral volume is the parameter most affected by the type of CTP postprocessing algorithm used, and particularly the deconvolution techniques used.
半影体积是受所使用的CTP后处理算法类型影响最大的参数,尤其是所使用的反褶积技术。
The SVD deconvolution method described is more subject to chronic ischemia or a tight carotid stenosis and therefore more likely to overcall the volume of the penumbra in this setting.
所描述的SVD去卷积方法更容易受到慢性缺血或颈动脉狭窄的影响,因此在这种情况下更可能覆盖半影的体积。
There are inherent microvascular abnormalities in white matter disease, including chronic hemodynamic in sufficiency in periventricular watershed zones and impaired blood-brain barrier permeability.37
白质疾病存在固有的微血管异常,包括心室周围分水岭区域的慢性血流动力学不足和血脑屏障通透性受损。37
All these can lead to per fusion abnormalities in areas of microvascular ischemia, which can create errors in the estimates of volume.
所有这些都可能导致微血管缺血区域的融合异常,从而在体积估计中产生误差。
Most of the fully automated software packages do not have adequate post processing tools to subtract the miscalculated volumes including skull base penumbral artifacts.
大多数完全自动化的软件包没有足够的后处理工具来减去计算错误的体积,包括颅底半影伪影。
There are tools in the manual (nonautomated) versions of CTP where an user can segment an region of interest around the artifactual penumbra and remove them from the calculation.
CTP的手动(非自动)版本中有一些工具,用户可以在人工半影周围分割感兴趣的区域,并将其从计算中删除。
Stroke mimics
Stroke mimics such as seizures, hypertensive encephalopathy, hemiplegic migraines causing vascular dysregulation, or vascular anatomy variations can also be falsely classified as ischemic penumbra.
中风模拟,如癫痫发作、高血压脑病、导致血管失调的偏瘫偏头痛或血管解剖变异,也可能被错误地归类为缺血性半影。
Seizures are a common stroke mimic, and CTP can demonstrate a continuum of findings depending on ictal vs postictal stage.
癫痫是一种常见的中风模拟,CTP可以根据发作期和发作后阶段显示一系列结果。
It is important to correlate perfusion abnormalities with clinical symptoms and CTA, as discordance between the CTP findings, clinical symptoms, and CTA findings provides an additional suggestion of diagnosis of a stroke mimic.
重要的是将灌注异常与临床症状和CTA相关联,因为CTP结果、临床症状与CTA结果之间的不一致性为中风模拟的诊断提供了额外的建议。
Perfusion in posterior circulation and lacunar infarcts
Although perfusion imaging has been well studied in anterior circulation, there is a dearth of evidence regarding appropriate thresholds and their utility in posterior circulation.
尽管灌注成像已经在前循环中得到了很好的研究,但缺乏关于适当阈值及其在后循环中的应用的证据。
However, accurate calculations of both ischemic core and penumbral volumes in the posterior fossa are limited by skull base and orbit artifacts.
然而,后颅窝缺血核心和半影体积的精确计算受到颅底和眼眶伪影的限制。
Furthermore, optimal perfusion thresholds for the posterior fossa circulation are not established.
此外,还没有建立后颅窝循环的最佳灌注阈值。
MRI-DWI has a clear advantage over CTP for lacunar infarcts and small watershed infarcts.
对于腔隙性梗死和小分水岭梗死,MRI-DWI比CTP具有明显优势。
MRP
DWI虽然是金标准,但是基于PWI的Tmax计算在定量问题上……
Compared with CTP, MR perfusion (MRP) is inherently less quantitative because the signal is not proportional to the concentration of contrast.
与CTP相比,MR灌注(MRP)本质上定量较少,因为信号与造影剂浓度不成正比。
Future directions
The current lack of standardization between CTP vendor software and postprocessing techniques may lead to variation in calculated core and mismatch.
当前CTP供应商软件和后处理技术之间缺乏标准化可能会导致计算核心的变化和不匹配。
Although automation has reduced human variability in CTP postprocessing, additional issues related to data acquisition and processing can lead to variable results, even when the exact same CTP raw data set is evaluated.
尽管自动化降低了CTP后处理中的人为可变性,但与数据采集和处理相关的其他问题可能会导致不同的结果,即使在评估完全相同的CTP原始数据集时也是如此。
There is a need for calibration while balancing intellectual property considerations.
需要在平衡知识产权考虑的同时进行校准。
The ideal standaridization would result in 2 similar patients with stroke being diagnosed with similar volumes of the infarct core and penumbra so that the same treatment decision is made independent of imaging modality, type of scanner, or postprocessing software.
理想的标准化将导致2名相似的中风患者被诊断为梗死核心和半影体积相似,因此,相同的治疗决策独立于成像模式、扫描仪类型或后处理软件。
Future work takes into consider ation broader physiologic and hemodynamic variables (i.e., a personalized approach).
未来的工作还需要采用多参数方法,结合Tmax、延迟图、CBF和CBV进行更准确的定量分析,同时考虑更广泛的生理和血流动力学变量(即个性化方法)。
Conclusion
Despite this inexact science, one can take comfort that there is some room for error, given the large treatment effects among those selected for treatment by the CTP imaging selection algorithms used in both the DAWN and DEFUSE 3 trials. However, with the surge of perfusion utilization in clinical decision making, the opportunity arises to standardize selection across software platforms and institutions to further improve and individualize patient selection and thereby improve clinical outcomes after acute ischemic stroke. This will require an aggressive and collaborative effort between the scientific community and industry partners to enhance future research, particularly for meta-analysis and data pooling.
尽管这是一项不精确的科学,但考虑到DAWN和DEFUSE 3试验中使用的CTP成像选择算法选择的治疗效果较大,人们可以放心地认为存在一定的错误空间。然而,随着临床决策中灌注利用率的激增,出现了跨软件平台和机构标准化选择的机会,以进一步改进和个性化患者选择,从而改善急性缺血性卒中后的临床结果。这将需要科学界和行业合作伙伴之间积极合作,以加强未来的研究,特别是荟萃分析和数据汇集。





![[操作系统笔记]基本分页存储管理](https://img-blog.csdnimg.cn/9f5288d6d9c5488891d8b5730ccbecca.png)
![[附源码]计算机毕业设计springboot物业管理系统](https://img-blog.csdnimg.cn/2ed124b3476242e2b26a08d95d027d13.png)



![洛谷千题详解 | P1019 [NOIP2000 提高组] 单词接龙【C++、Java语言】](https://img-blog.csdnimg.cn/74ba48b1a27f40729548fb1892d28383.png)