Title
题目
Screening Outcomes of Mammography with AI in Dense Breasts: A Comparative Study with Supplemental Screening US
《乳腺密度高的女性中,使用AI辅助的乳腺X线筛查与补充筛查超声的比较研究》
Background
背景
Comparative performance between artificial intelligence (AI) and breast US for women with dense breasts undergoing screening mammography remains unclear.
人工智能(AI)与乳腺超声在乳腺密度高的女性进行乳腺X线筛查时的比较表现仍不明确。
Method
方法
A retrospective database search identified consecutive asymptomatic women (≥40 years of age) with dense breasts who underwent mammography plus supplemental whole-breast handheld US from January 2017 to December 2018 at a primary health care center. Sequential reading for mammography alone and mammography with the aid of an AI system was conducted by five breast radiologists, and their recall decisions were recorded. Results of the combined mammography and US examinations were collected from the database. A dedicated breast radiologist reviewed marks for mammography alone or with AI to confirm lesion identification. The reference standard was histologic examination and 1-year follow-up data. The cancer detection rate (CDR) per 1000 screening examinations, sensitivity, specificity, and abnormal interpretation rate (AIR) of mammography alone, mammography with AI, and mammography plus US were compared.
一项回顾性数据库搜索识别出连续的无症状女性(年龄≥40岁,乳腺密度高),她们在2017年1月至2018年12月期间在一家初级医疗中心接受了乳腺X线检查及补充的全乳手持超声检查。五名乳腺放射科医生分别进行了单独乳腺X线检查和借助AI系统的乳腺X线检查的连续阅片,并记录了他们的召回决定。从数据库中收集了乳腺X线检查与超声联合检查的结果。一位专门的乳腺放射科医生复审了单独乳腺X线检查或与AI辅助检查的标记,以确认病灶的识别。参考标准为组织学检查和1年随访数据。比较了单独乳腺X线检查、AI辅助乳腺X线检查以及乳腺X线检查加超声的每千次筛查中的癌症检出率(CDR)、敏感性、特异性和异常解释率(AIR)。
Conclusion
结论
Although AI improved the specificity of mammography interpretation, mammography plus supplemental US helped detect more node-negative early breast cancers that were undetected using mammography with AI.
尽管AI提高了乳腺X线检查解读的特异性,但乳腺X线检查加补充超声能够检测出更多未被AI辅助乳腺X线检查发现的淋巴结阴性早期乳腺癌。
Results
结果
Among 5707 asymptomatic women (mean age, 52.4 years ± 7.9 [SD]), 33 (0.6%) had cancer (median lesion size, 0.7 cm). Mammography with AI had a higher specificity (95.3% [95% CI: 94.7, 95.8], P = .003) and lower AIR (5.0% [95% CI: 4.5, 5.6], P = .004) than mammography alone (94.3% [95% CI: 93.6, 94.8] and 6.0% [95% CI: 5.4, 6.7], respectively). Mammography plus US had a higher CDR (5.6 vs 3.5 per 1000 examinations, P = .002) and sensitivity (97.0% vs 60.6%, P = .002) but lower specificity (77.6% vs 95.3%, P < .001) and higher AIR (22.9% vs 5.0%, P < .001) than mammography with AI. Supplemental US alone helped detect 12 cancers, mostly stage 0 and I (92%, 11 of 12).
在5707名无症状女性(平均年龄52.4岁 ± 7.9岁)中,33例(0.6%)确诊为癌症(中位病灶大小为0.7厘米)。与单独乳腺X线检查相比,AI辅助乳腺X线检查具有更高的特异性(95.3% [95% CI: 94.7, 95.8], P = .003)和更低的异常解释率(AIR)(5.0% [95% CI: 4.5, 5.6], P = .004),而单独乳腺X线检查的特异性为94.3% [95% CI: 93.6, 94.8],AIR为6.0% [95% CI: 5.4, 6.7]。乳腺X线检查加超声检查的癌症检出率(CDR)更高(每千次筛查5.6 vs 3.5, P = .002),敏感性也更高(97.0% vs 60.6%, P = .002),但特异性较低(77.6% vs 95.3%, P < .001),且AIR较高(22.9% vs 5.0%, P < .001),与AI辅助的乳腺X线检查相比。仅使用补充超声检测出了12例癌症,其中大部分为0期和I期(92%,即12例中的11例)。
Figure
图
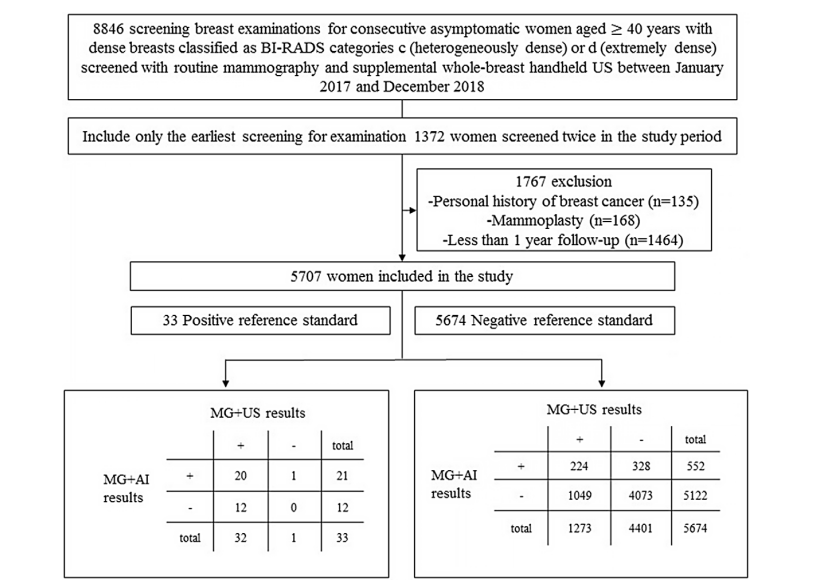
Figure 1: Flowchart shows study inclusion and exclusion. AI = artificial intelligence, BI-RADS = Breast Imaging Reporting and Data System, MG = mammography.
图1: 流程图显示了研究的纳入和排除标准。AI = 人工智能,BI-RADS = 乳腺影像报告与数据系统,MG = 乳腺X线检查。
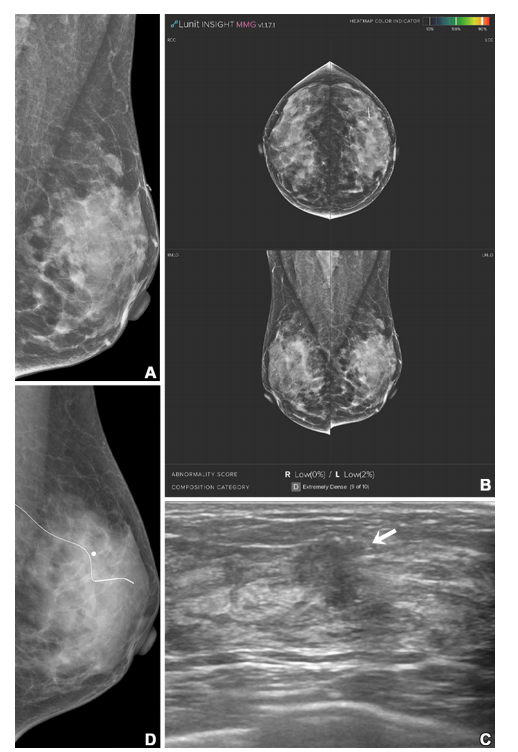
Figure 2: Imaging in a 51-year-old woman with extremely dense breasts (Breast Imaging Reporting and Data System category d). (A, B) Left mediolateral oblique digital mammogram (A) and right and left craniocaudal (RCC, LCC) and right and left mediolateral oblique (RMLO, LMLO) mammograms with artificial intelligence (Lunit INSIGHT MMG, version 1.1.7.1; Lunit) (B) show no abnormality. The radiopaque bar marker, which is attached on the skin to mark a previous benign fibroadenoma excision site, is visible. (C) Supplemental transverse US image shows a 1.2-cm irregular mass (arrow) in the left breast. (D) Left mediolateral oblique digital mammogram after US-guided wire localization shows no suspicious findings, even in retrospect. The radiopaque round marker, which is attached on the skin to mark the wire insertion site, is visible. The patient was treated with breast-conserving surgery, and the mass was proven to be invasive ductal carcinoma (pT1N0, 1.5 cm in size, estrogen receptor and progesterone receptor positive, human epidermal growth factor receptor 2 negative, histologic grade 1).
图2: 影像显示一名51岁乳腺极其致密的女性(乳腺影像报告与数据系统分类d)。(A, B) 左侧中斜位数字乳腺X线照片 (A) 和右侧及左侧头尾位 (RCC, LCC) 以及右侧及左侧中斜位 (RMLO, LMLO) 乳腺X线照片 (B) 使用人工智能(Lunit INSIGHT MMG,版本1.1.7.1;Lunit)辅助显示未见异常。附着在皮肤上的不透明标记条可见,用于标记之前良性纤维腺瘤切除手术的部位。(C) 补充横断面超声图像显示左乳房有一个1.2厘米的不规则肿块(箭头)。(D) 超声引导下的导丝定位后的左侧中斜位数字乳腺X线照片在回顾时仍未显示可疑发现。附着在皮肤上的不透明圆形标记可见,用于标记导丝插入部位。患者接受了乳腺保留手术,肿块被证实为浸润性导管癌(pT1N0,大小1.5厘米,雌激素受体和孕激素受体阳性,HER2阴性,组织学等级为1)。
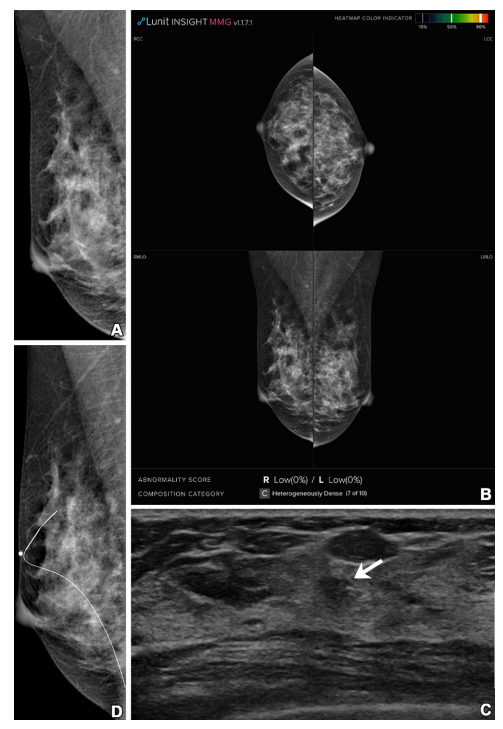
Figure 3: Imaging in a 41-year-old woman with heterogeneously dense breasts (Breast Imaging Reporting and Data System category c). (A, B) Right mediolateral oblique digital mammogram (A) and right and left craniocaudal (RCC, LCC) and right and left mediolateral oblique (RMLO, LMLO) mammograms with artificial intelligence (Lunit INSIGHT MMG, version 1.1.7.1; Lunit) (B) show no abnormality. (C) Supplemental transverse US image shows a 1.0-cm irregular mass (arrow) in the right breast. (D) Right mediolateral oblique digital mammogram after US-guided wire localization shows no suspicious findings, even in retrospect. The radiopaque round marker, which is attached on the skin to mark the wire insertion site, is visible. The patient was treated with breast-conserving surgery, and the mass was proven to be invasive ductal carcinoma (pT1N0, 0.7 cm in size, estrogen receptor and progesterone receptor positive, human epidermal growth factor receptor 2 negative, histologic grade 1).
图3: 影像显示一名41岁乳腺结构异质性致密的女性(乳腺影像报告与数据系统分类c)。(A, B) 右侧中斜位数字乳腺X线照片 (A) 和右侧及左侧头尾位 (RCC, LCC) 以及右侧及左侧中斜位 (RMLO, LMLO) 乳腺X线照片使用人工智能(Lunit INSIGHT MMG,版本1.1.7.1;Lunit)辅助 (B) 显示未见异常。(C) 补充横断面超声图像显示右乳房有一个1.0厘米的不规则肿块(箭头)。(D) 超声引导下的导丝定位后的右侧中斜位数字乳腺X线照片在回顾时仍未显示可疑发现。附着在皮肤上的不透明圆形标记可见,用于标记导丝插入部位。患者接受了乳腺保留手术,肿块被证实为浸润性导管癌(pT1N0,大小0.7厘米,雌激素受体和孕激素受体阳性,HER2阴性,组织学等级为1)。
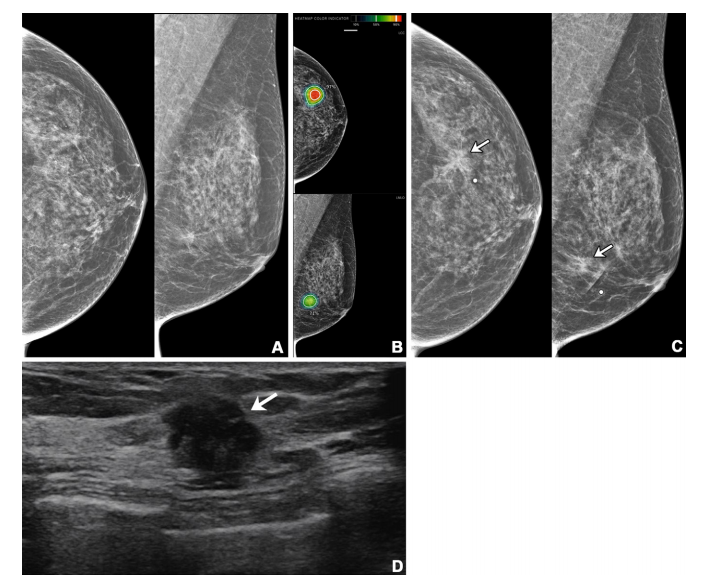
Figure 4: Imaging in a 56-year-old woman with heterogeneously dense breasts (Breast Imaging Reporting and Data System category c). (A) Left craniocaudal (left) and mediolateral oblique (right) digital mammograms show no abnormality. (B) Left craniocaudal (LCC, top) and left mediolateral oblique (LMLO, bottom) mammograms with retrospectively applied artificial intelligence (AI) (Lunit INSIGHT MMG, version 1.1.7.1; Lunit) show the lesion was given abnormality scores of 97% and 71%, respectively. The color bar indicates pixel-level abnormality scores corresponding to heatmap contour lines. Breast US performed the same day was considered negative (not shown). (C) Left craniocaudal (left) and mediolateral oblique (right) digital mammograms acquired 9 months later show an irregular mass (arrows) in the left breast, which correlates with the heatmap areas scored as 97% and 71% by AI in the earlier screening mammogram (B). The radiopaque round marker denotes the site of the palpable abnormality indicated by the patient. (D) Transverse US image shows an irregular mass (arrow) in the left breast. The patient was treated with breast-conserving surgery, and the mass was proven to be invasive lobular carcinoma (pT2N1, 2.5 cm in size, estrogen receptor and progesterone receptor negative, human epidermal growth factor receptor 2 positive, histologic grade 3).
图4: 影像显示一名56岁乳腺结构异质性致密的女性(乳腺影像报告与数据系统分类c)。(A) 左侧头尾位(左)和中斜位(右)数字乳腺X线照片显示未见异常。(B) 左侧头尾位 (LCC, 上) 和左侧中斜位 (LMLO, 下) 乳腺X线照片在回顾时应用人工智能(AI)(Lunit INSIGHT MMG,版本1.1.7.1;Lunit)分析后,显示病灶分别被赋予97%和71%的异常评分。颜色条表示与热图轮廓线对应的像素级异常评分。同一天进行的乳腺超声检查被认为是阴性(未显示)。(C) 9个月后获取的左侧头尾位(左)和中斜位(右)数字乳腺X线照片显示左乳房有一个不规则肿块(箭头),与早期筛查乳腺X线照片 (B) 中AI赋予97%和71%评分的热图区域相对应。不透明圆形标记表示患者指出的可触及异常位置。(D) 横断面超声图像显示左乳房内有一个不规则肿块(箭头)。患者接受了乳腺保留手术,肿块被证实为浸润性小叶癌(pT2N1,大小2.5厘米,雌激素受体和孕激素受体阴性,HER2阳性,组织学等级为3)。
Table
表
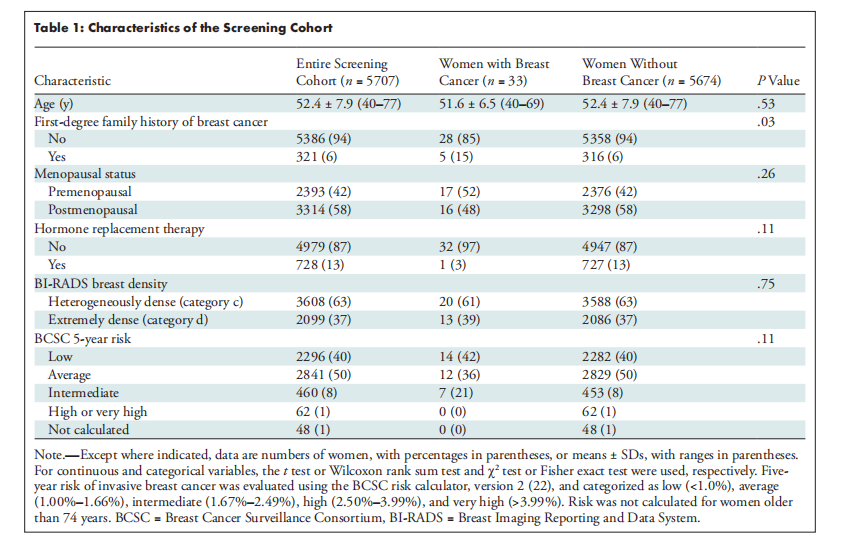
Table 1: Characteristics of the Screening Cohort
表1: 筛查队列的特征
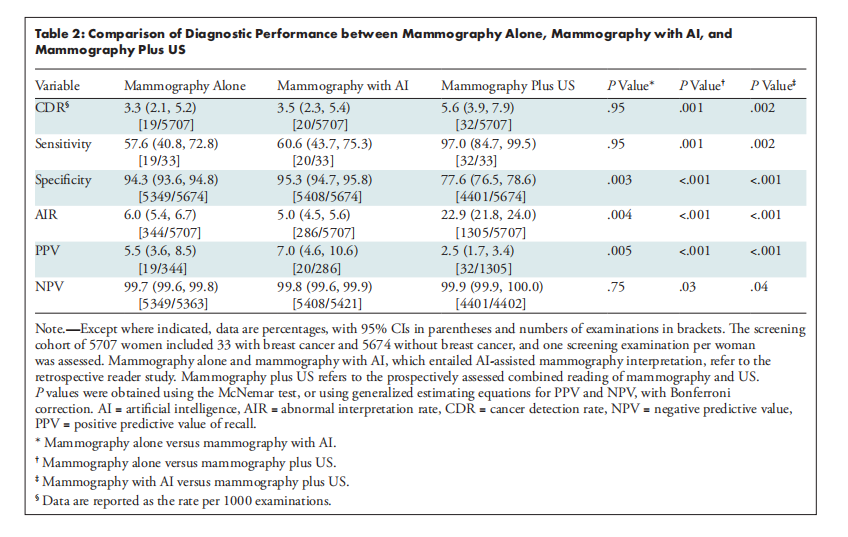
Table 2: Comparison of Diagnostic Performance between Mammography Alone, Mammography with AI, and Mammography Plus US
表2: 单独乳腺X线检查、AI辅助乳腺X线检查与乳腺X线检查加超声的诊断性能比较
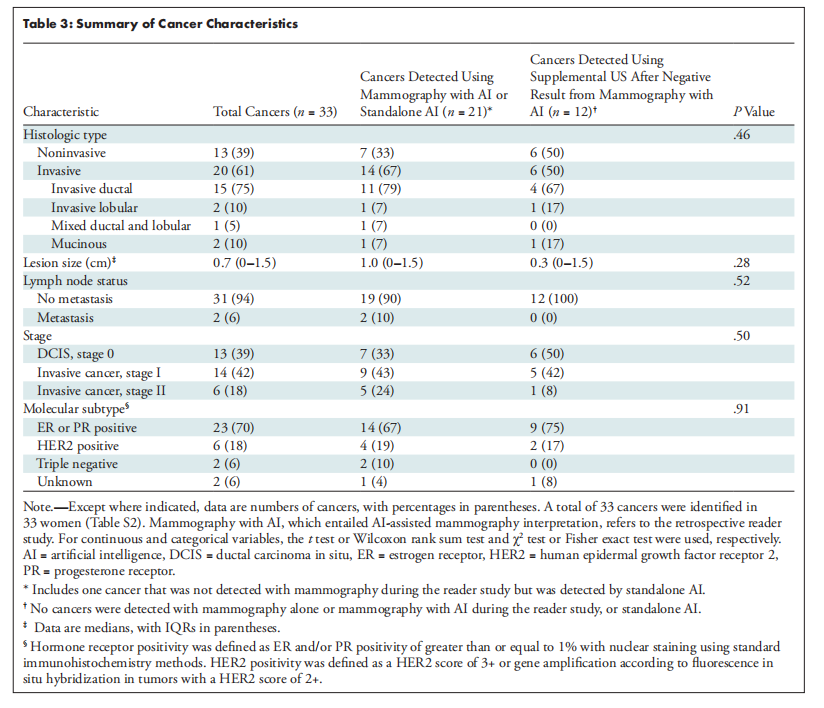
Table 3: Summary of Cancer Characteristics
表3: 癌症特征汇总


















